Gut reactions
When I first started learning about herbalism and holistic medicine, I came across the adage ‘all disease begins in the gut.’ This has been attributed to Hippocrates, who lived in the 5th century BC and is often referred to as the father of modern medicine—though I’ve since been interested to learn that much of what was attributed to him was likely not from the man himself, but rather the whole school of thought around medicine that he helped to found. Regardless, it’s a bold statement.
This idea didn’t compute for me at the time I heard it; my view of the body and health didn’t place our gut in such a central place of importance—I was trained as a neuroscientist, after all. But the more I learn, but more I can get on board with this suggestion, at least when it comes to chronic disease and systemic inflammation.
To help make sense of this, let’s look at the gut as more than just the place you break down and assimilate your food. (Although there’s quite a lot to say about just that!) If you think about it, our gastrointestinal system is actually continuous with the outside world. Imagine if you could shine a light into your mouth and the photons didn’t absorb into your tissue, they would travel all the way through the esophagus, stomach, and intestines and out the other end (making a unique flashlight indeed). Because of this, some have described our bodies as a kind of elongated doughnut, with the doughnut hole being our GI tube. So the inside (of our gut) is kind of the outside (of our body).
Perhaps it’s not surprising, then, that the lining of our gut is similar in many ways to our skin, in that it provides protection, allows for secretion and absorption, and serves as a critical barrier to moderate what passes through into the rest of the body. In fact, these two tissues—gut lining and skin—are both made of epithelial cells, and derived from the same embryonic cell layer, so their similarities are no coincidence!
Also just like the skin, our gut lining plays a key role in sensory perception. While this may seem an odd idea, we can actually think of the gut as one of our major sense organs, just as important as the eyes, ears, nose, mouth, and skin in helping us to know what’s in our environment and how to respond appropriately. The gut senses the outside world through the food that we consume, which is giving it information not only about available nutrients, but also any toxins to be avoided in the future, or pathogens to be cleared. It’s also intimately linked with our nervous system, and has a strong impact on our minds and emotions. The more we learn about this gut-brain axis, the more we see how the term “gut feelings” ins’t just a metaphor.
From the standpoint of our immune system, ingesting food is actually a pretty dangerous action we undertake many times each day. What a convenient avenue for pathogens to get into our bodies and find a new home! This inherent vulnerability is likely why the immune system is deeply interwoven into our gut lining, allowing it to detect any intruders and mount a defensive response. Connections between the gut and immune system is an exciting new area of study and much remains to be learned, but one thing that’s shifted my understanding of integrated bodily function is how the gut lining can also be viewed as modified lymph (immune) tissue. In fact, when I started digging into the literature on all of this, a statement in one review paper really grabbed me: “The GI tract is considered the largest immunologic organ in the body.” That’s quite a shift from how I learned it! But maybe Hippocrates and other ancient systems of medicine were onto this long ago.
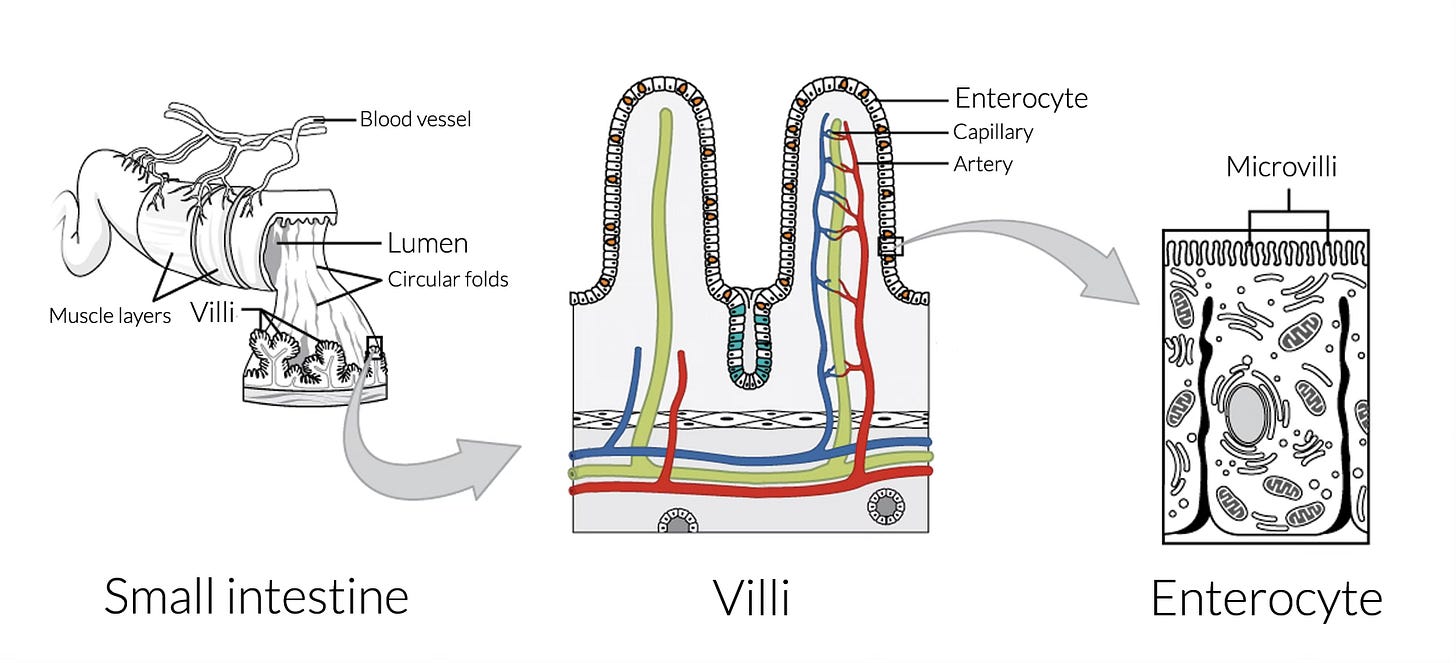
To see why the gut is also an immune organ, we need to take a closer look at its anatomy. If we hitch a ride on an endoscope and take a journey down into your small intestine, we find the inside of the tube (called the lumen) is lined with villi, or finger-like projections, that serve to massively increase the area of the absorptive surface of the gut lining. And lining each of these villi are tightly packed cells called enterocytes, each of which has even more (and tinier) microvilli on their surface. Think SpongeBob SquarePants with a toothbrush on his head. (Welcome to my brain.) Overall, it’s been estimated that if you could flatten out a healthy human gut lining, the surface area would be more than 30 square meters! That’s about 15 times larger than the surface of our skin, and a lot of real estate packed into a small part of our bodies—all to maximize our chances of absorbing nutrients.
Those enterocytes are doing a lot more than increasing surface area, however. Their tightly packed arrangement is critical for our health. Connected to their neighbors by ‘tight junctions’ and other very cool interlocking protein connectors, the barrier that is formed by the enterocytes regulates what gets into our bodies and what stays in the gut to be excreted. A healthy barrier allows in properly broken down food and nutrients, and keeps out pathogens, toxins, and larger food fragments.
However, the tight junctions between the enterocytes are regulated too. They can become more or less permeable depending on many factors. The list of things that can compromise the integrity of our gut lining seems to grow with each new study, and includes environmental factors (e.g., chemical pollutants, detergents, microplastics, pathogens), dietary factors (e.g., food allergens, high sugar, pro-inflammatory oils, alcohol, gluten, vitamin/mineral deficiency), other physiological factors (e.g., stress, microbiome disruption, medication like antibiotics or NSAIDs, poor sleep) and of course genetic factors.
When the junctions between enterocytes get more permeable than they should be, that’s what’s known as ‘leaky gut’—aptly named, because your gut lining becomes more like a sieve, letting all kinds of molecules and micro-organisms pass through, which can cause a lot of havoc in your body.
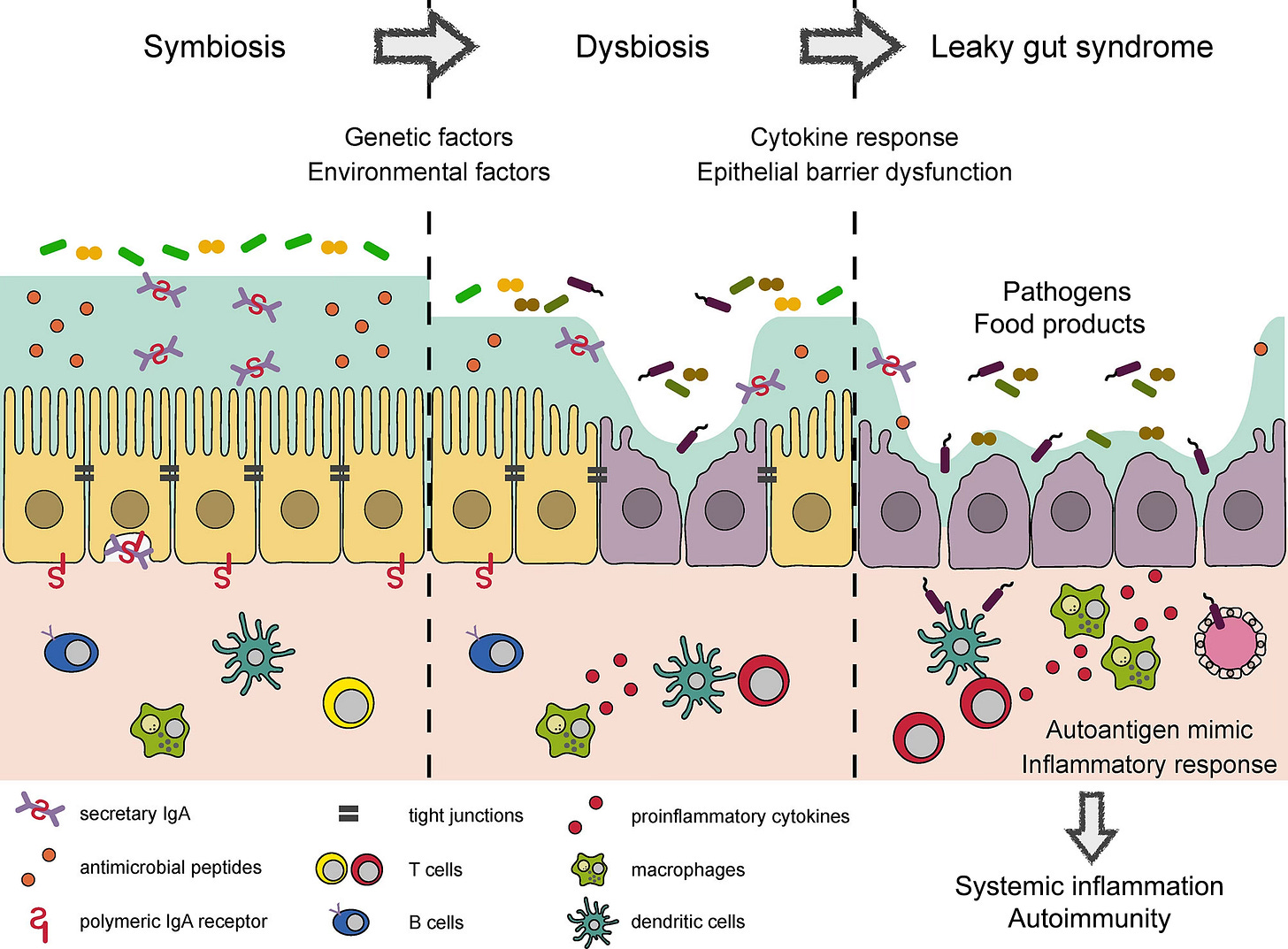
This is where the tie to systemic inflammation comes in. I mentioned that the gut lining is kind of like lymph tissue—that’s because it has immune components squeezed right up in there along with the enterocytes, as well as in the protective mucous layer above the enterocytes, and in the tissue below it that contains blood vessels. This makes your body able to very efficiently mount an immune attack should anything unwanted get past the barrier. I’ll spare you (and let’s be real, myself) the details of the many cell types and molecules involved in immune responses, but suffice to say that we have all the immune components we need right there in the gut lining not only for a local inflammatory response in the intestines, but for a systemic inflammatory response, where immune messages are carried through the bloodstream to all parts of the body.
When low-grade, local inflammation in the gut goes on too long, your immune system can decide that this threat isn’t going away, and it’s time to pull out the big guns and go systemic. Systemic inflammation is a wonderful thing when you have a major infection—it’s basically your immune system on high alert, rapidly creating cells and antibodies that are targeted to find the invaders and neutralize them, as well as more general inflammatory molecules that kill pathogens… and cause collateral damage to your own tissues in the process. Things get a little messy, but it’s more important to clear the pathogen and stay alive.
Ideally, this whole response is meant to be acute: deal with a threat and then return to baseline and clean up the damage. But in today’s world, we’re all exposed regularly to at least some of those factors that disrupt our gut integrity, so systemic inflammation seems to be increasingly common—and when it’s chronic, the body never gets a chance to clean up the damage. I’ve written before about the prevalence of systemic inflammation and its links to most of the chronic diseases we face today. And the fact that it can be—and likely often is—initiated in our gut feels super important to get our heads around.
What can systemic inflammation look like? Well, since it can affect most any system of the body, and will often leverage existing vulnerabilities or weak spots, it can look very different for different people. You may not have full blown chronic disease or autoimmunity, but there are many common, less severe presentations that are also signs of systemic inflammation. Here are some examples of how inflammation can show up around the body:
musculoskeletal & connective tissue: joint pain, muscle tension/soreness/weakness
nervous system: irritability, anxiety, depression, brain fog, dizziness, migraines & other headaches, tinnitus, ataxia/motor issues
skin: eczema, hives, psoriasis, other rashes
cardiovascular system: high cholesterol, atherosclerosis (Fun fact: cholesterol is like a molecular band-aid, which the body applies to inflammatory damage inside the blood vessels. So high cholesterol isn’t the ‘problem’ per se—it’s the body’s attempt at a solution to inflammation!)
respiratory system: chronic phlegm, congestion, cough
endocrine system: hormonal imbalance, menstrual cycle irregularity, severe PMS, hair loss, sleep disruption
digestive system: gas, bloating, constipation, diarrhea, cramping, gut pain
That kind of seems like a laundry list of everything that can go wrong, doesn’t it? Well, exactly. In my own body, I’ve had 10+ of those symptoms at various times, especially as I’ve entered perimenopause, and I can tell you that except for the digestive issues, I’d never have thought that any of this was related to my gut health. But making major changes to my diet and working on healing my gut has improved or eliminated all of them.
I’m definitely not saying that in every case for every person these things are 100% due to compromised gut permeability—so to say that ‘ALL disease begins in the gut’ is too broad a statement—but for me it was a game-changer to start seeing these symptoms under one larger umbrella of systemic inflammation, rather than a whole bunch of disconnected issues in my body. It took me years to really grasp this. If you’re experiencing a handful of these kinds of symptoms, it’s worth attending to the gut as one of the primary drivers of the problem.
Viewed one way, all of this can seem super complex and daunting: TONS of things cause leaky gut, and then leaky gut can cause TONS of problems! But I prefer to view this as an exciting opportunity for healing: there are so many points of entry to begin improving the state of our guts. And it’s also encouraging to know that the gut can be a powerful place to focus our healing efforts, since through its central role in regulating inflammation, it can impact widespread aspects of our health.
Healing the Gut
Thankfully, there are many ways we can begin to heal our guts, and this is an area where holistic medicine shines. The biggest levers of change at our disposal are nothing flashy or magical, but basic lifestyle changes that are often simple (if not always easy). Move more. Reduce stress as much as you can. Get serious about sleep hygiene. Explore your diet carefully and identify factors that could be contributing to impaired gut health. Across the board factors here include significantly reducing added sugar, refined carbs, and problematic oils, and limiting alcohol intake. Make sure you’re getting adequate vitamin D and zinc. There will be other dietary factors specific to each person that require deeper inquiry—identifying food intolerances, for example, which (spoiler alert) are much more common than we think. All of this is the kind of holistic medicine I’m super grateful to be training in, so I’m really looking forward to being able to work with folks 1:1 to develop individualized strategies for all of these approaches.
And of course, there are the plants! Herbs can help with all of the avenues above, including movement, stress management, sleep, and providing needed minerals while helping calm inflammation. For the digestive tract specifically, a ‘gut heal’ tea is one of the herbalist’s go-to medicines. Many plants are valuable here; my preferred base blend includes: chamomile (flower), calendula (flower), plantain (leaf), marshmallow (leaf), and ginger (root). You can mix and match these to your taste or depending on what you have available, but in general this formula provides wound-healing, warming digestive, moistening, and soothing anti-inflammatory actions. Other common additions include peppermint, fennel, licorice, meadowsweet, catnip… If you’re working with an herbalist, they can also customize this blend to your constitution and symptoms. A quart of this tea daily is usually the recommended starting dose (see my previous post for tips on making tea).

I will add that in today’s world, we often want the ‘quick fix.’ Pharmaceutical medicine has trained us to expect this (even though many of those approaches only address surface symptoms). But to really heal the underlying issues, you have to do the harder lifestyle work—there’s no way around it. In this case, if you just drink gut heal tea and keep doing everything else that’s harming the gut, the herbs will only be band-aid medicine. We want to address the root.
Thinking back to Hippocrates, it turns out that attending to medical philosophy from 2500 years ago can serve us well in modern times. There’s a reason why gut healing is a central tenet of herbal medicine—it (still) works.
Peripheral
I barely touched on the incredible world of the microbiome in this post, but of course it’s a major player in gut health. I had the privilege to speak with leading microbiome researcher Emeran Mayer on the Mind & Life podcast. My favorite part is when I asked him about the gut-brain connection, and the gut being referred to as the ‘second brain.’ His response was a total light bulb moment!
Happily, I’ve started working at my local amazing herb shop, The Elderberry. 🎉🌿 I’m learning so much, and am beyond thrilled to be part of the stellar team there! They’re just starting up an Herb of the Month Club, which I’ll be joining for sure—I think it’ll be a great way for folks to gain more experience with herbs in a low-key hands-on way, with an intimate community, one herb at a time. The group meets online twice/month. I’d love to see you there!
One of my favorite things in life is having my worldview totally upended. This happened recently when I listened to the Telepathy Tapes podcast series. It’s about non-speaking autistic folks and the gifts that they have… but more broadly it’s about consciousness and the nature of this world we live in. The show is controversial on a number of levels, but I think it’s well worth a listen.